“The Six-Month Dispensation model came at the right time. Now, I can spend more time on my farm and don’t have to explain so often why I go to the hospital.”
— Arlindo Nalili, patient at 17 de Setembro Health Facility
In the heart of Zambézia Province, many families confront the daily reality of living with HIV while striving to maintain their livelihoods amid scarce resources. Until late 2024, clinically stable patients typically returned to health facilities every one to three months for antiretroviral therapy (ART) refills – a rhythm that imposed long journeys, lost wages, and the quiet toll of stigma in tight-knit communities.
At that time, only seven health facilities in the province had begun implementing Six-Monthly Medication Dispensation (6MMD), which reduces routine clinical visits from as many as twelve per year to just two. This simple yet transformative change provided patients like Manuel Albano the freedom to focus on their families, farms, and futures rather than spending considerable amounts of time waiting to receive clinical services at busy health facilities. But scaling it across a province as large and varied as Zambézia demanded buy-in from national, provincial, and district managers, nurses and pharmacy technicians, data clerks, and community advocates alike.
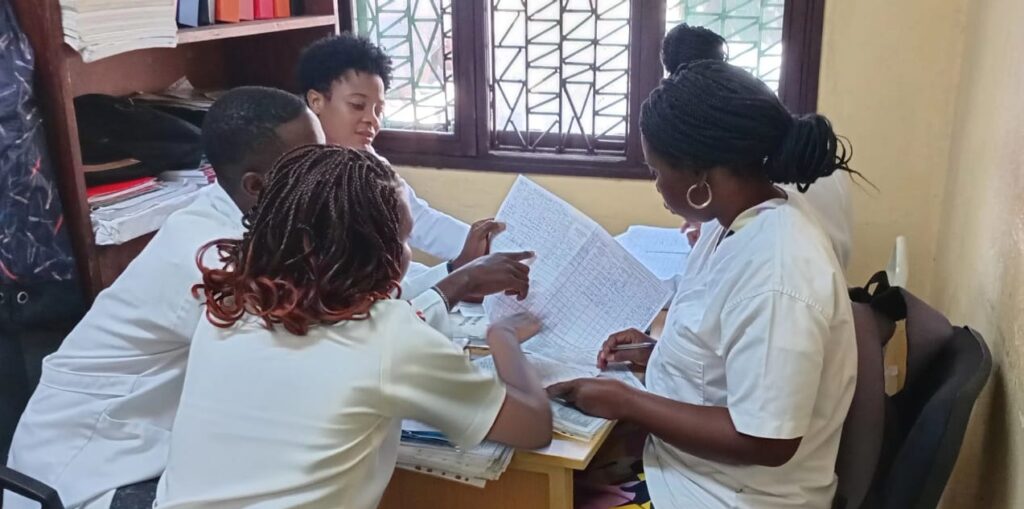
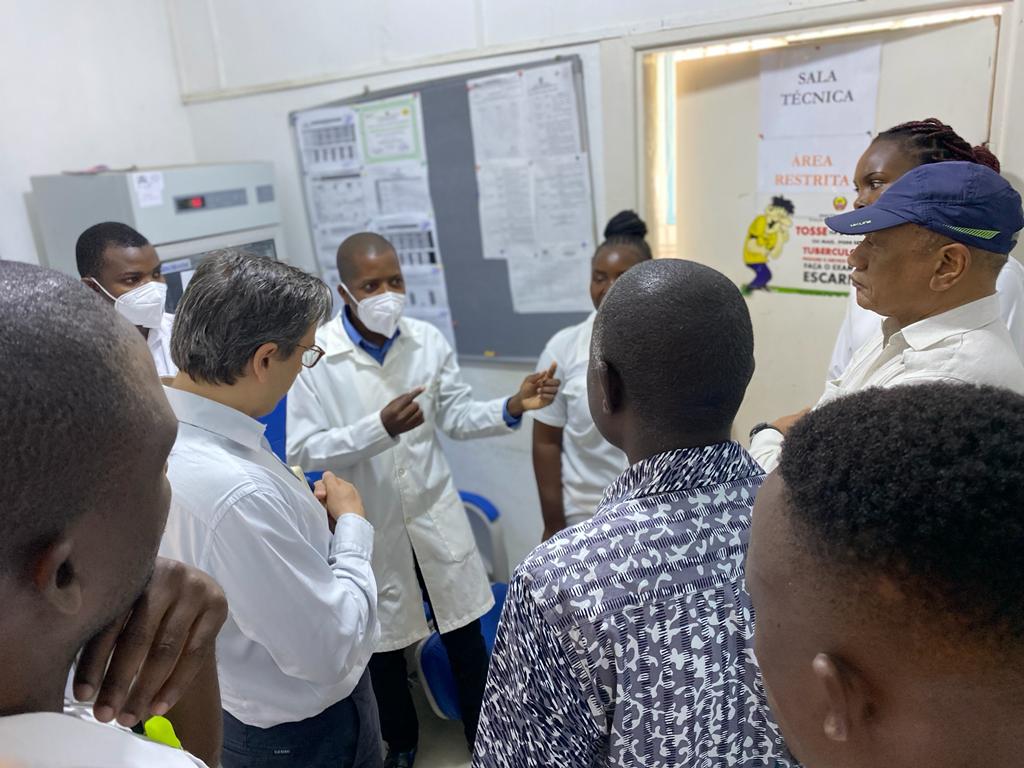
Acknowledging the potential, the Ministry of Health approved a coordinated expansion strategy in October 2024. Led by the Zambézia Province Health Directorate (DPSZ) with support from C-Saúde, district health officers and C-Saúde mentors organized intensive workshops on the 6MMD guidelines, paired with hands-on exercises in updating master cards and using the patient-tracking database to flag eligible clients. Weekly virtual check-ins and monthly in-person supervisory visits provided troubleshooting and encouragement, while data managers helped facilities generate automatic reports on uptake rates and stock levels, enabling rapid course corrections whenever bottlenecks emerged.
Community engagement proved equally vital. At the 17 de Setembro Health Facility in Quelimane, a multisectoral task force comprising local activists, traditional leaders, and clinic staff hosted interactive health talks, where patients asked questions, shared concerns, and heard testimonials from early adopters. Posters and radio spots in local languages and Portuguese emphasized that six-monthly medication refills were not a reduction in care but a recognition of patients’ stability, granting them autonomy and dignity. In the rural Mocubela Sede Health Facility, community health committees invited patients to “come with a friend” during enrollment days, pairing newcomers with peers who had already experienced the convenience of longer dispensing intervals.
Between October 2024 and June 2025, these efforts bore fruit. The number of supported facilities surged from seven to 37, covering most of the province’s districts. Province-wide coverage of 6MMD among eligible clients nearly doubled, from nine percent at baseline to 20 percent by the end of the reporting period, by which time more than 79,000 clients were enrolled in 6MMD. At 17 de Setembro, more than 72% of eligible patients opted in as workflows shifted to accommodate dedicated ART pick-up days and data clerks ensured accurate enrollment tracking. Even in Mocubela Sede, where infrastructure challenges once loomed large, 70% of stable patients now enjoy six-monthly medication refills.
The impact extended beyond the numbers. Nurses reported a smoother outpatient flow, with fewer ART pickups per clinic day, allowing them to provide more focused counseling for newly enrolled or complex patients. Pharmacy technicians, once pressed by constant dispensing demands, found time to conduct inventory reconciliations and provide adherence support. Patients described feeling less like clinic visitors and more like empowered partners in their own care, able to sow fields, attend market days, and participate in community events without the dilemma of frequent hospital trips.
Looking ahead, provincial health authorities and C-Saúde, through CDC/PEPFAR support, are committed to improving access to six-monthly drug dispensation in all supported health facilities that meet the necessary structural and staffing criteria by December 2025. Plans include scaling up mobile supervision and technical support teams to reach the most remote sites, integrating real-time performance dashboards at the district level, and deepening partnerships with community networks to sustain demand and address emerging patient concerns.
For patients like Manuel Albano, who can now tend to his crops without the monthly trek to the clinic, six-monthly drug dispensation is more than a program, it is a gateway to normalcy, productivity, and hope. As Mozambique continues its journey toward epidemic control, differentiated service delivery approaches such as this offer a blueprint for balancing clinical rigor with human dignity, transforming the way HIV care is delivered across rural landscapes and urban centers alike.